COVID-19 ProtocolsLearn More
Covid-19 Safe Environment - CDC Guidelines In Place - Learn MoreBook Release Announcement - The Hernia Solution, 2nd Edition - Click here for more information
Need help? Call us 626.584.6116
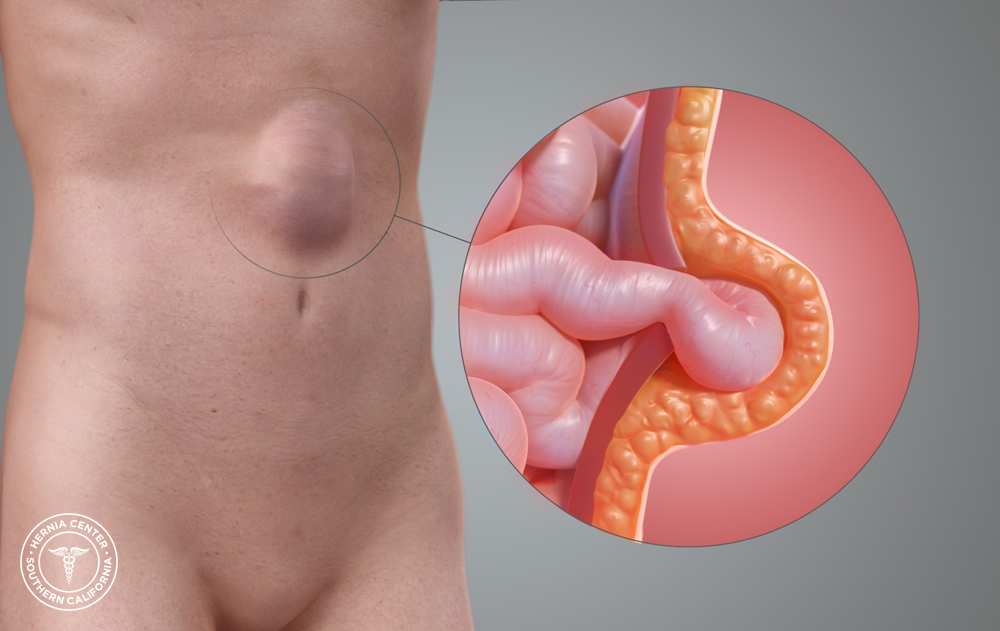
A ventral hernia is a bulge protruding through an opening in the abdominal wall, typically as a result of a tear or division in the muscles or fascia. Based on where they occur, ventral hernias can be classified into different subtypes:
If you think you have a ventral hernia and wish to seek treatment, the Hernia Center of Southern California can help. Having collectively performed over 15,000 hernia surgeries, Dr. David Albin and Dr. Michael Albin are well-recognized experts in abdominal / ventral hernia repair. They specialize in all types of advanced open and laparoscopic techniques, including the Albin Tension Free Mesh Technique—an internationally recognized advanced version of the standard Tension Free Mesh Technique that was developed exclusively for the Hernia Center of Southern California by Dr. David Albin.
To learn more about abdominal / ventral hernias and their treatment, we invite you to continue reading the information below, or simply contact us today to book a consultation with one of our board-certified hernia surgeons.
When the abdominal muscles and fascia lose integrity, hernias may form. The abdomen is subjected to normal pressures and forces that allow us to walk upright, lift, and carry, as well as maintain proper placement of our internal organs. When such forces occur over areas of inherent weakness—such as the umbilicus or a prior incision—damage in the thin muscle fibers may accumulate over time. When enough of the fibers are torn, a hole can form. Our normal abdominal pressure then pushes our internal contents out the hole, through the path of least resistance. This is similar to a pressurized pipe that springs a leak. Your internal organs, however, cannot completely leave your body because the skin, fat, and other surrounding structures prevent their expansion. Over time, these tissues can stretch and the hernia can increase in size. This results in an abdominal hernia. This process occurs more rapidly when the body is subjected to more excessive forces such as those that occur with heavy lifting and straining. In some circumstances, the tissues are weaker than normal, and hernias develop sooner. This can occur in smokers or with certain genetic conditions.
Conditions that put excessive tension on the abdominal wall:
Conditions that weaken the integrity of tissues:
An abdominal / ventral hernia can be asymptomatic (meaning there are no obvious symptoms), but the most common reason that people seek treatment is because they develop discomfort at or around the affected area. The discomfort is usually worsened when there is an increase in intra-abdominal pressure. This occurs with heavy lifting, straining, or prolonged standing. Pain tends to worsen by the end of the day, especially after a full day of strenuous activity. Surrounding muscular inflammation may also result in pain near the site of the hernia. The pain is usually made better with rest. Pain levels can vary from minor intermittent discomfort to more significant constant pain.
In some circumstances, the pain is unrelenting and severe. In those instances, emergent evaluation at a hospital is recommended, as there is a possibility of hernia incarceration. An incarcerated hernia may be associated with nausea, vomiting, and non-reducible firmness over the area.
Other secondary symptoms that may be associated with abdominal / ventral hernias include:
Some people use medications to help with mild to moderate symptoms. This includes over-the-counter anti-inflammatories, Tylenol, and ice application. Other people use support devices such as abdominal binders and hernia belts. While these may help to improve comfort, surgical treatment is the only way to definitively improve symptoms.
Since the hernia is the result of a physical tear or hole in the muscles and fascia of the abdomen, it cannot heal on its own. In most cases, the greatest risk of delaying repair is worsening symptoms and increasing hernia size. Occasionally ventral / abdominal hernias become incarcerated. This occurs when the contents that push through the hernia exceed what can freely fit through the defect. When this occurs, the hernia cannot be easily reduced and becomes incarcerated. The increased pressure may reduce blood flow to the trapped hernia contents, posing risk for strangulation—also known as lack of oxygenated blood flow—or intestinal obstruction. Both situations need to be addressed emergently by either manual reduction or surgery. When strangulation occurs, if manual reduction does not occur in a matter of hours, then emergency surgery may be the only option due to a greater likelihood of tissue death of the trapped contents.
An abdominal / ventral hernia can be diagnosed by a physician during physical examination. The hallmark is the presence of a bulge on the abdominal wall that may or may not be reducible. Radiographic imaging is not always necessary to diagnose an abdominal / ventral hernia. If the diagnosis is uncertain, then an ultrasound, CT scan, or MRI may be performed. If you have been diagnosed with an abdominal / ventral hernia, you should consult a hernia specialist.
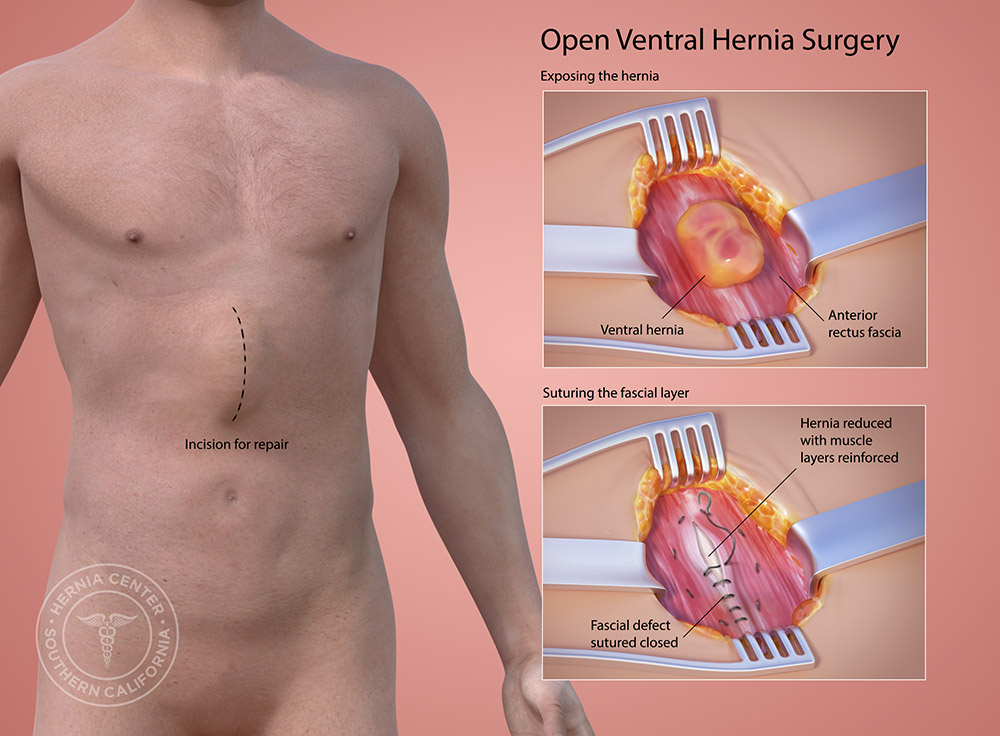
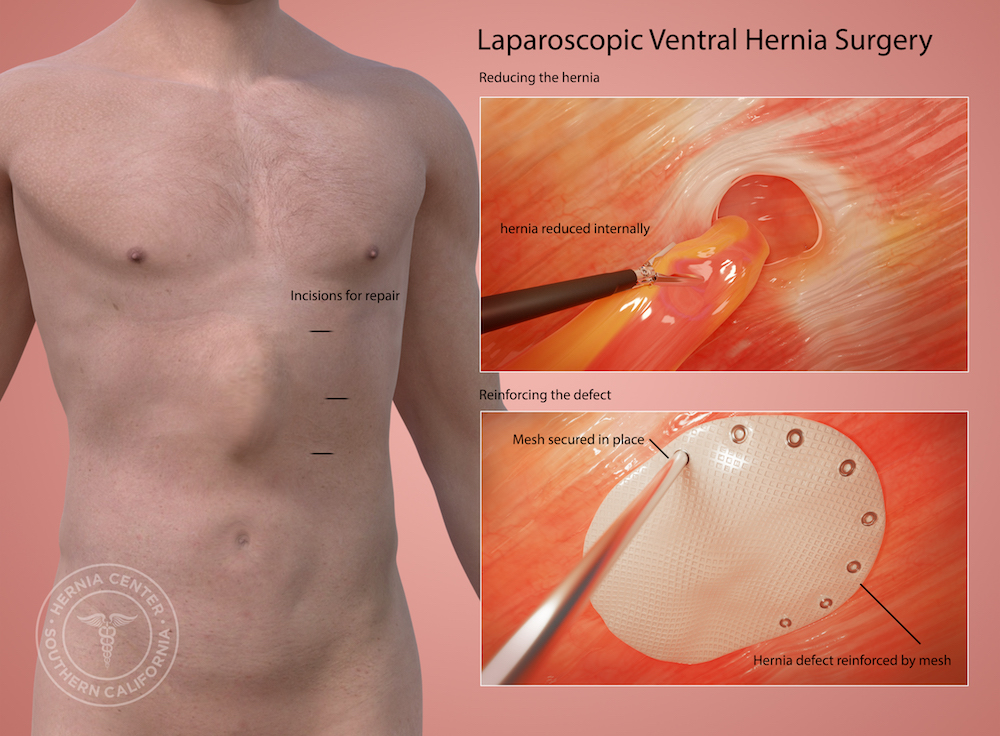
At the Hernia Center of Southern California, we repair abdominal / ventral hernias using the “tension-free” mesh technique. Abdominal / ventral hernia repair can be performed as a same-day, outpatient procedure under a local anesthesia with sedation. We also perform abdominal / ventral hernia repairs using laparoscopy, which requires a general anesthetic.
During abdominal / ventral hernia repair, the mesh is placed behind the weakness or hole in the abdominal wall. The mesh is tailored to extend past the edges of the hernia. This ensures the mesh will act as a sturdy platform for all new tissue growth, as well as supports the existing abdominal wall muscle. Muscles are never cut, and nothing is sutured together to cause tension. The polypropylene mesh is thin and incredibly flexible throughout the healing process to incorporate safely into the muscle wall.
Surgery time varies, but most small to medium sized hernias can be repaired in around an hour. Surgical time can increase depending on additional factors such as hernia size, obesity, or previous surgery. With our technique of local anesthesia with sedation, surgery is often pain-free with no discomfort during the immediate recovery.
Physical activity is an important part of abdominal / ventral hernia surgery recovery. We encourage unrestricted walking the day after surgery with gradual incorporation of cardiovascular exercise starting 5–7 days after surgery, followed by light weightlifting at the gym starting 2 weeks after surgery. Patients that are physically active before and after surgery tend to have a faster recovery and a quicker resolution of post-operative discomfort. No matter the technique of repair that is used, there is always a certain amount of post-operative pain and discomfort after surgery. The pain usually starts in the evening of the day of surgery and peeks at around 72 hours. For this time period, your surgeon will provide a prescription pain medication. Non-opiate alternative pain relievers are encouraged. After the first 72 hours, there is still pain and discomfort, but it is more associated with muscular soreness and stiffness. For this we recommend the use of over-the-counter anti-inflammatories and ice application when resting and both before and after physical activity. Physical activity significantly reduces the duration of mechanical soreness and stiffness associated with the recovery. One month after surgery, the soreness is much milder and less frequent. While the surgical repair is strong at this point and can tolerate most heavy lifting, the occasional use of over-the-counter anti-inflammatory or ice application is usually all that is necessary for pain relief. Most people are resuming regular activity 4–6 weeks after surgery, and the stiffness and soreness usually completely dissipates over a 3 month period.
We recommend light meals and plenty of hydration during the first 24 hours following your surgery. For the first week, a fiber diet including fruits and vegetables is recommended as there may be a change in bowel habits during this period. Constipation is not unusual during the first week if prescription pain medication is taken.
Most people return to sedentary work in anywhere from a few days to a week after surgery, light-lifting work in around 1–2 weeks after surgery, and full-lifting duty around 4–6 weeks after abdominal / ventral hernia surgery.